What is Medication Reconciliation?
- Explain the concept of medication reconciliation
- Describe the goal of medication reconciliation
Introduction to Medication Reconciliation Video
This brief introductory video (4:35 minutes) was created by ISMP Canada for Safer Healthcare Now! (SHN!). SHN! is a national campaign aimed at improving the safety of patient care through learning, sharing and implementing interventions such as medication reconciliation that are known to reduce avoidable adverse events.
In order to see this video, you must have javascript available and the Adobe Flash Player.
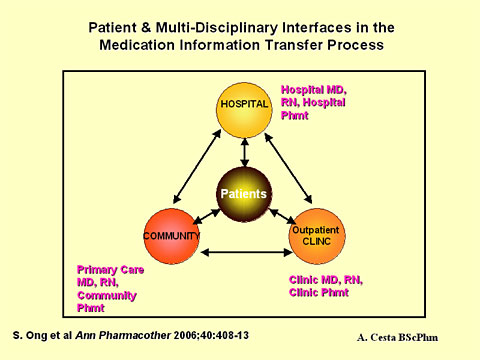
Medication Reconciliation is a formal process in which healthcare providers partner with patients and their families to ensure accurate and complete medication information transfer at interfaces of care. This includes admission and discharge from a hospital or changes in care setting, service, or level of care.
From: Wong, Jacqueline D. Bajcar, Jana M. Wong, Gary G. Alibhai, Shabbir M H. Huh, Jin-Hyeun. Cesta, Annemarie. Pond, Gregory R. Fernandes, Olavo A. Medication reconciliation at hospital discharge: Evaluating discrepancies. Annals of Pharmacotherapy. 42(10):1373-9, 2008 Oct.
The Medication Reconciliation Process
The process of medication reconciliation involves the following key components:
- Obtaining the most complete and accurate list possible of the patient’s current regularly taken medications, known as the Best Possible Medication History (BPMH).
- Using the BPMH when writing admission, transfer and discharge medication orders.
- Comparing the BPMH with the admission, transfer or discharge medication orders, identifying and bringing any discrepancies to the attention of the team and, if appropriate, making changes to the orders and documenting all changes.
Goal of Medication Reconciliation
The ultimate goal of medication reconciliation is to prevent adverse drug events (ADEs) at all interfaces of care (admission, transfer and discharge), for all patients. The aim is to eliminate undocumented intentional discrepancies and unintentional discrepancies by reconciling all medications, at all interfaces of care.
An undocumented intentional discrepancy occurs when the prescriber (usually the physician) intentionally adds, changes or discontinues a medication the patient was taking prior to admission but this is not clearly documented in the patient’s medical record.
An unintentional discrepancy occurs when the prescriber (usually the physician) unintentionally changes, adds or omits a medication the patient was taking prior to admission.
Preventing of Medication Errors
Types of medication errors that can be prevented by reconciling medications may include:
- failure to prescribe clinically important home medications while in hospital
- incorrect doses or dosage forms
- missed or duplicated doses resulting from inaccurate medication records
- failure to clearly specify which home medications should be resumed and/or discontinued at home after hospital discharge
- duplicate therapy at discharge (result of brand/generic name combinations or hospital formulary substitutions)
Examples of Medication Reconciliation
Example of an Undocumented Intentional Discrepancy
A patient receiving atenolol for hypertension was admitted for surgery. The admitting resident did not order atenolol on admission due to concerns about perioperative hypotension. The reason for not ordering atenolol was not documented in the medical record. The patient was discharged on the third postoperative day and was given a discharge prescription that did not include atenolol. The patient was unsure whether to resume treatment with atenolol at home and called her family doctor for advice. The family doctor called the patient’s surgeon to clarify the discrepancy. The surgeon did not know why the atenolol was stopped while in hospital and called the hospital pharmacy. The pharmacy did not have a record of the change so the pharmacist on the surgical unit tried to contact the admitting resident but the resident was no longer on the service.
Examples of an Unintentional Discrepancy
- An elderly woman was admitted to a general medicine unit with a diagnosis of community-acquired pneumonia. Antibiotics and symptom management were ordered and started. Two days later the patient had a myocardial infarction and it was found that a beta-blocker (cardiac medication) had been unintentionally omitted on admission.
- A patient was admitted for total knee replacement surgery. After four or five days the patient was not motivated and refused to get out of bed. The family mentioned to the nurse that the patient had been on an antidepressant medication prior to admission and it had not been ordered while in hospital. The medication was ordered. It took approximately one week for the medication to work again, resulting in a prolonged hospital stay.
Exercise
This excercise is also available as a PDF.
Think about the patient most recently admitted to your service and answer the following questions:
- Did the patient or family bring their medications to the hospital?
- Were the medications properly labeled and stored in their original containers or a medication compliance aid (e.g., dosette)?

- Did the patient have a medication list?
- Was the list from another healthcare provider or was it written by the patient?
- Did you have to contact the patient’s family doctor or pharmacist to clarify something about their medications?
- What information did you need and were you able to get it?
Self-test
Why is it necessary to reconcile medications?
-
To obtain a complete list of medications the patient is regularly takingThis is ONE reason for reconciling medications. Obtaining a complete list of medications the patient was regularly taking prior to admission ensures that a full assessment of the patient's drug therapy can be completed and reduces the chance that a medication will be missed when the patient is discharged.
-
To reduce adverse drug eventsThis is ONE reason for reconciling medications. Adverse drug events commonly occur as a result of incomplete reconciliation of medications when patients are admitted, transferred or discharged from the hospital. This may be due to an unintended omission, duplication, or drug interaction.
-
To ensure the patient is receiving appropriate drug therapyThis is ONE reason for reconciling medications. The purpose and dosage of each medication must be known to ensure that patients are receiving appropriate drug therapy.
-
All of the aboveThis is the CORRECT answer! A complete and accurate list of medications is essential to reduce preventable adverse drug events and ensure that patients are receiving appropriate drug therapy at all times.
Answer: D
Summary
Medication Reconciliation is a process designed to prevent medication errors at all interfaces of care (admission, transfer and discharge). It involves three steps:
- Obtaining the most complete and accurate list possible of the patient’s regularly taken home medications.
- Using the list when writing medication orders.
- Comparing the list with the patient’s admission, transfer or discharge orders, identifying and bringing any discrepancies to the attention of the team and, if appropriate, making changes to the orders and documenting all changes.

