Article
Chronic non-cancer pain is an expensive and growing problem within
industrialised countries. In a 1998 review, the
Marinker (1998), in a discussion of concordance versus compliance,
cited studies indicating that when there is congruence between service
providers’ and service users’ beliefs about treatment, concordance is higher.
Patient concordance with treatment is inextricably connected with the
individual’s perception of whether the intervention is relevant, meaningful and
likely to be successful (Kotarba and Seidel 1984, Donovan and Blake 1992,
Schussler 1992, Yardley and Furnham 1999). The treatment endorsement patterns
of both service providers, like occupational therapists, and service users need to be identified and compared.
Participants in the study attributed a range of negative effects
to physicians’ disbelief of their pain. These effects included: growing
self-doubt, increasingly unsupportive family members, inaccurate information
going to employers, frustration over feeling that the physicians did not listen
to them, and the perception that physicians disbelieved their pain. Eccleston
et al (1997) compared a composite group of 60 physicians’ and patients’
understandings of the causes of chronic pain. This study revealed that while
common categories of belief emerged (blame, responsibility and the need to
protect identity), the two groups did not share common beliefs within those
classifications.
Aim of the study
The Pain Society (British and Irish Chapter of the International
Association for the Study of Pain) identified occupational therapists as important
members of the treatment team in its report, Desirable Criteria for Pain Management Programmes (Pain Society 1997). It follows that the issues discussed above
are of relevance to occupational therapy and require closer examination. This
paper presents the occupational therapist findings that have been extracted from
the results of an ongoing much larger multidisciplinary study, examining
service providers’ and service users’ congruence of beliefs regarding specific treatments for chronic
pain.
The literature and websites related to chronic pain intervention
were reviewed and all the identified treatment components were listed. The
resultant list of 63 treatment components formed the basis of a questionnaire
(see Table 1 for the items included). This list was presented in random order
within the questionnaire so that respondents would not be influenced by
researcher-identified categories. The questionnaire section of interest in this
report asked respondents to identify which treatment components they personally
endorsed as needed or not needed for people withchronic pain.
Participants and procedure
The board of the National Occupational Therapy Pain Association
gave its permission to survey the membership (93 therapists at the time of the
study) and provided mailing labels. The members were informed in the covering
letter that return of the questionnaire would be taken as consent to
participate. The participants were also invited to volunteer for a follow-up
phase of the larger research project and requested to provide contact
information if they were interested. Because of this, in eight cases it was
possible to return questionnaires to participants for additional information
where sections had been omitted or misunderstood.
Findings
Of the 93 questionnaires, 44 (47.3%) were returned. There were 41
women and 3 men, whose ages ranged between 28 and 60 years (mean = 41 years)
and years in practice between 1 and 31 years (mean =14 years). The most commonly
reported type of pain-related work was with mixed caseloads (n = 33, 75%), followed by work with people having
pain related to orthopaedic conditions (n = 8, 18.2%). The respondents showed a
wide range in hours of undergraduate training, with 34 (77.3%) reporting that
they had received 0 hours of training in pain and pain management. Only 3 (6.8%) of the total group had received more
than 15 hours of pain education as undergraduates. At a continuing professional
development (CPD) level, although 7 (15.9%) therapists reported having only 10 hours
or less of additional training, 29 (65.9%) had participated in over 30 hours of
pain-related CPD.
Organising therapists’ beliefs about treatment components
The range of treatment components that therapists ranked as needed
or not needed was grouped into five general categories: (A) Education for
self-management, (B) Health care professional applied biomedical interventions,
(C) Health care professional applied psychosocial interventions, (D)
Facilitation of peer-support network and (E) Complementary therapies. A panel
of occupational therapy lecturers at the
BPCQ scores
The respondents reported higher rates of endorsement for beliefs
around internal (IS) factors as influencing pain, followed by chance happening
(CH) and an overall low belief in powerful doctors (PD). In comparison with Skevington’s
(1990) findings for these subscales with nonpatients, marked differences are
evident in the PD and CH scores (Table 2). Because Skevington’s (1990) figures
are not normative, the two groups can only be compared for the purpose of
provoking discussion; no statistically significant relationship is implied.
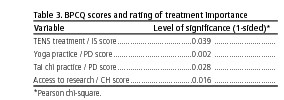
BPCQ scores were divided into categories of ‘high’ and ‘low’, with the mean score used as the divide for ranking. Chisquare analysis of the high/low BPCQ scores and therapists’ beliefs that each individual treatment component was needed or not needed served to highlight several interesting trends. Statistically significant findings, as detailed in Table 3, emerged for the treatment components of TENS (transcutaneous electrical neuromuscular stimulation), yoga, tai chi and client access to research findings. Therapists who scored high on the IS (internal factors) scale in the BPCQ tended to see the use of TENS as a needed treatment for chronic pain (p = 0.039). Therapists who scored high in PD (powerful doctor) tended to believe that the yoga (p = 0.002) and tai chi (p = 0.028) treatment options were needed. The analysis also revealed that therapists who scored high on CH (chance happening) were more likely to endorse that people with pain needed access to research findings (p = 0.016).

Study limitations
There are several key limitations to the findings presented. Only 44
of the possible 93 (47.3%) questionnaires were returned, so the sample is less
than ideal and no claims of representativeness should be inferred. Because the
respondents could choose to be anonymous and there were financial restraints,
no follow-up of non-respondents could be carried out. Therefore, it was not
possible to determine demographic characteristics that might have influenced
participation in the study. Also, the respondents, because of their membership
in the National Occupational Therapy Pain Association, should be viewed as a
sub-specialty group of occupational therapists that may have a wider knowledge and
experience base in chronic pain than other occupational therapists.
Lastly, survey data do not capture the full range of responses
possible in exploring a complex area such as pain. This postal survey focused
on ‘what’ occupational therapists endorse and provided predominately
quantitative data. However, without a follow-up examination of ‘why’ the therapists held these preferences, interpretation can only be
incomplete and speculative at best. The second, qualitative stage of this
research is currently being designed.
Discussion and conclusion
This survey has provided a preliminary profile of a group of
occupational therapists’ beliefs in relation to chronic pain treatments. There
was a wide range in respondents’ years of experience and hours of CPD training
related to chronic pain. Most of the therapists worked with clients from a
mixture of diagnostic groups, and nearly 75% of all the therapists
participating in this study had received no dedicated training on pain during
their undergraduate education. The study
respondents appeared to be a heterogeneous group of therapists, each
bringing a unique blend of training and experience to his or her practice. This lack
of consistency was mirrored in what individual therapists felt were necessary
treatments for chronic pain, although a definite trend was evident in the
categories of treatment that the therapists tended to endorse more uniformly.
The therapeutic interventions related to Education for self-management were found to be more consistently identified as needed for treatment. It is possible that this is partially a function of the high amount of CPD that the therapists engaged in. Also, this may be related to the profession’s core philosophy of enabling occupation. According to Law (1997, p2), ‘enabling occupation means collaborating with people to choose, organise and perform occupations which people find useful or meaningful in a given environment’. Self-management approaches to chronic pain are evidently one such enabling tool that occupational therapists are well prepared to facilitate.
A potential explanation for another of the study’s findings may lie in the combination of this focus on enabling, the profession’s philosophical roots of client-centredness (Law and Baptiste 1995, Sumsion 2000) and the concept of occupational competence (Matheson and Bohr 1997). The BPCQ scores reflected that the National Occupational Therapy Pain Association group of occupational therapists tended to believe less strongly in the idea of a ‘powerful doctor’ (or other health care professional) and in ‘chance happening’ than non-patients from other studies (Skevington 1990). Occupational therapists ascribe to a belief system that people have mastery in their own lives and are not controlled by random fates.
The study produced some less easily understood findings,
particularly in light of the above-mentioned beliefs. As identified, there was
a positive relationship between high BPCQ scores in the ‘powerful doctor’ (PD)
category and endorsement of yoga (p = 0.002) and tai chi (p = 0.028). While it may be argued that it is in keeping with occupational
therapists’ philosophy of client-centredness to support lifestyle choices for
complementary therapies (such as tai chi and yoga), it was puzzling that this
endorsement was found within the subgroup of respondents (31.8%) who scored high in their belief in ‘powerful doctors’. Although the
majority of respondents did not strongly endorse ‘powerful doctors’, the
findings seem to suggest that there may be a subgroup of therapists that is
supportive of alternative interventions focusing on a client-centred definition
of ‘useful’, while at the same time still operating within a medical model
endorsing the concept of professional expertise.
Two features of current health care may offer some insight into
this apparent contradiction. First, most occupational therapists, as
demonstrated in the findings of this and other studies (Scudds and Solomon
1995, Unruh 1995, Rochman 1998, Strong et al 1999), have a paucity of
undergraduate education and training in pain. This may leave them poorly
equipped to formulate an evidence-based argument for the pain interventions
that they provide and/or endorse. Although the therapists did report a high
rate of CPD in chronic pain, this expertise is acquired over time.
The question of whether practice and beliefs change with CPD is
only now beginning to be addressed within the discipline (Jones et al 2000).
Often working within large hospital-based services and multidisciplinary teams,
therapists may adopt the values of other team members whose professional
underpinnings and treatment approaches are theoretically grounded in biomedical
reductionism (Freeman et al 2000). In this scenario, it would be possible to
see an occupational therapist as swaying between the influences of the
team milieu and his or her professional tenets.
A second consideration in exploring these unexpected findings is
that health care practitioners are subject to the social forces in which the
health care service is provided. Recently, Weinblatt and Avrech-Bar (2001)
challenged occupational therapists to develop a questioning attitude towards what they traditionally hold to be ‘truths’ about science
and medicine. They proposed that occupational therapists need to understand how
postmodernism challenges commonly held modernist beliefs that health care consists
of universal truths and principles explained through scientific analysis. In postmodernist thinking, there are no universal
givens and personal reality changes in relation to the sociopolitical, temporal
and environmental contexts in which an individual lives (Siahpush 1998). The
emerging social phenomenon in western cultures of challenging biomedicine’s
superiority has seen a growing exploration and endorsement of interventions
that previously were held to be from the fringe and ‘alternative’ (Hodgkin
1996, Raithatha 1997, Siahpush 1998). The findings of this study, where
50%-79% of occupational therapists stated that they believed interventions such
as acupuncture, yoga and meditation to be needed for the treatment of chronic
pain, lend some degree of support to this idea.
Weinblatt and Avrech-Bar (2001) emphasised that occupational therapy is well positioned to offer interventions from within both traditional science driven models (such as biomechanics and exercise physiology) and methods that reflect a postmodern redefinition of health based on individual perceptions, beliefs and values. The profession’s client-centred philosophy allows occupational therapists to work flexibly with a variety of clients, each of whom defines his or her own ‘truth’. The findings of this survey, where therapists support traditional biomedical constructs at the same time as endorsing ‘alternative’ interventions (such as yoga), may cautiously be interpreted as lending support to Weinblatt and Avrech-Bar’s (2001) proposition. As discussed above, this survey only examined the ‘what’ of occupational therapists’ beliefs. Stronger evidence-based interpretation cannot go forward until the ‘why ‘ is added to the equation. Occupational therapy is only beginning to deal with the philosophical issues of constructivism and postmodernism and this paper makes no claims related to either paradigm. The introduction of these terms should be seen rather as a provocation, to stimulate and perhaps even aggravate the reader into further discourse.
Much more research is obviously needed. A qualitative second stage
to this study is now in development to explore what explanation occupational
therapists themselves bring to their decision making about chronic pain
interventions. Chronic pain is a complex and life-altering condition. Occupational
therapists, by virtue of their unique philosophical background, have much to
offer to people with chronic pain. The challenge now is for occupational therapists
to be willing to explore their own beliefs and attitudes while they seek a
shared understanding of pain and treatment interventions with the clients that they serve.
Acknowledgements
This study would not have been possible without the financial
support of the Constance Owens Trust; the willing participants from the
National Occupational Therapy Pain Association members; my research
supervisors, Professor A Jacoby (Department of Primary Care, University of
Liverpool) and Dr G Baker (Walton Neurological Centre); Dr Maria Leitner
(Director of Research, School of Health Sciences, University of Liverpool); and
my academic colleagues’ supportive but critical perspectives. My particular appreciation
to the thoughtful comments and guidance of the anonymous BJOT reviewers.
Thank you all
References
Bates MS, Rankin-Hill L, Sanchez-Ayendez M (1997) The effects of
the cultural context of health care on treatment of and
response to chronic pain and illness. Social Science and Medicine, 45, 1433-47.
Chapman SL, Jamison RN, Sanders S (1996) Treatment helpfulness questionnaire:
a measurement of patient satisfaction with
treatment modalities provided in chronic pain management programmes. Pain,68,
349-61.
Donovan J,
Donovan MI, Evers K, Jacobs P (1999) When there is no benchmark: designing
a primary care-based chronic pain management
programme from the scientific basis up. Journal of Pain and Symptom Management,
18(1), 38-48.
Eccleston C, Williams AC, Stainton Rogers W (1997) Patients’ and professionals’
understandings of the causes of chronic pain:
blame, responsibility and identity protection. Social Science and Medicine, 45(5), 699-709.
Fields HL (1995) Core curriculum for professional education in pain: a report of
the Task Force on Professional Education
of the International Association for the Study of Pain.
Freeman M,Miller C, Ross N (2000) The impact of individual
philosophies of teamwork on multi-professional practice and the
implications for education. Journal
of Interprofessional Care, 14(3), 237-47.
Hodgkin P (1996) Medicine, postmodernism and the end of certainty.
British Medical
Journal, 313(7072), 568-69.
Jones D, Ravey J, Steedman W (2000) Developing a measure of beliefs
and attitudes about chronic non-malignant pain: a pilot
study of occupational therapists. Occupational Therapy International, 7(4), 232-45.
Kotarba JA, Seidel JV (1984) Managing the problem pain patient: compliance
or social control? Social Science
and Medicine, 19, 1393-1400.
Law M (1997) Core concepts in occupational therapy. In: E
Townsend, ed. Enabling occupation: an occupational
therapy perspective.
Law M, Baptiste S (1995) Client-centred practice: what is it and
does it make a difference? Canadian
Journal of
Occupational Therapy, 62, 250-57.
LeFort SM, Gray-Donald K, Rowat KM, Jeans ME (1998) Randomised controlled
trial of a community-based psychoeducation programme
for the self-management of chronic pain. Pain, 74(2-3), 297-306.4
Maniadakis N, Gray A (2000) The economic burden of back pain in
the
Marinker M (1998) Compliance is not all. British Medical Journal, 316(7125), 150-51.
McQuay HJ, Moore RA, Eccleston C, Morley S,Williams AC (1997) Systematic
review of outpatient services for chronic pain
control. Health Technology
Assessment, 1(6), 1-135.
Pain Society (1997) Desirable criteria for pain management programmes.
Raithatha N (1997) Medicine, postmodernism and the end of certainty.
Postmodern philosophy offers a more appropriate system
for medicine. British Medical Journal,
314(7086), 1044.
Rathbun CR, Slate JR (1995) Lack of comparability of two pain
locus of control measures. Assessment
in Rehabilitation
and Exceptionality, 2(3), 153-61.
Rochman DL (1998) Students’ knowledge of pain: a survey of four schools. Occupational Therapy International, 5(2), 140-54.
Rochman DL, Herbert P (1999) Rehabilitation professionals’ knowledge and attitudes survey
regarding pain.
Schussler G (1992) Coping strategies and individual meanings of
illness. Social Science and
Medicine, 34(4), 427-32.
Scudds R, Solomon P (1995) Pain and its management: a new pain curriculum
for occupational therapists and physical
therapists. Physiotherapy
Seers K, Friedli K (1996) The patients’ experiences of their
chronic non-malignant pain. Journal
of Advanced Nursing,
24, 1160-68.
Siahpush S (1998) Postmodern values, dissatisfaction with
conventional medicine and popularity of alternative therapies. Journal of Sociology, 34(1), 58-70.
Skevington SM (1990) A standardised scale to measure beliefs about
pain control (BPCQ): a preliminary study. Psychology and Health, 4, 221-32.
Spence A (1999) Services
for people with pain.
Strong J, Tooth L, Unruh A (1999) Knowledge about pain among newly
graduated occupational therapists: relevance for curriculum
development. Canadian Journal of
Occupational Therapy, 66(5), 221-28.
Sumsion T (2000) Client-centred practice: the challenge of
reality. OT Now, July/August, 22-23.
Turk DC (1996) Biopsychosocial perspectives on chronic pain. In:
RJ
Turnquist K, Engel J (1994) Occupational therapists’ experience
and knowledge of pain in children. Physical and
Occupational Therapy in Pediatrics, 14, 35-51.
Unruh A (1995) Teaching student occupational therapists about
pain: a course evaluation. Canadian
Journal of
Occupational Therapy, 62(1), 30-36.
Von Korff M, Moore J, Lorig K, Cherkin DC, Saunders K, Gonzalez
VM, Laurent D, Rutter C, Comite F(1998) A randomised
trial of a layperson led self-management group intervention for back pain
patients in primary care. Spine, 23(23), 2608-15.
Vrancken MA (1989) Schools of thought on pain. Social Science and Medicine, 29(3), 435-44.
Weinblatt N, Avrech-Bar M (2001) Postmodernism and its application
to the field of occupational therapy. Canadian Journal of Occupational Therapy,
68(3), 164-70.
Yardley L, Furnham A (1999) Attitudes of medical and non-medical students
toward orthodox and complementary
therapies: is scientific evidence taken into account? Journal of Alternative and Complementary
Medicine, 5(3), 293-95.
Author
Cary A Brown, MA, OTM(C), SROT, Lecturer, Division of Occupational
Therapy, University of Liverpool, Johnston Building, Brownlow Hill, Liverpool
L69 3GB.