Article
Disability and Rehabilitation, 2005; 27(14): 849 – 861
The
use and impact of assistive devices and other environmental modifications
on everyday activities and care in young
children with cerebral palsy
SIGRID
ØSTENSJØ1, EVA BROGREN CARLBERG2,
& NINA K. VØLLESTAD3
1Faculty
of Health Sciences, Oslo University College, 2Department
of Woman and Child Health, Karolinska Institute, Stockholm, Sweden, and 3Institute
of Nursing and Health Sciences, University of Oslo, Norway
Purpose:
The study describes use of assistive devices and other environmental
modifications, and their impact on everyday activities and care in young
children with cerebral palsy (CP).
Method:
Ninety-five children (55 boys, 40 girls; mean age 58 months, SD 18 months) and
their parents were studied using a cross-sectional design. The Pediatric
Evaluation of Disability Inventory (PEDI) was applied to assess daily
activities using the three measurement scales: functional skills, caregiver
assistance, and modifications of the environment. Use of modifications was described
related to the five severity levels of the Gross Motor Function Classifications
System (GMFCS). Impact was rated on the Caregiver Assistance scale of the PEDI
and on a five-point Likert scale.
Results: Out
of the 1075 provided environmental modifications, 980 were in regular use to
support mobility, self-care and social function among 84 children. The number
increased with GMFCS levels; children at levels IV and V used 80% of the
modifications, with large variations between the children at same level. Adaptations
of housing and transportation facilitated effective use of assistive devices.
Half of the parents rated the modifications to have moderate to very large
effect on the child’s mobility, 25% on self-care skills, and 20% on social
function. Furthermore, 65% reported that the modifications lightened the
caregiving for mobility, 75% for self-care and 25% for social function.
Functional independence and care demands often benefited from different types
of modifications.
Conclusion: The
variations in use and benefits of environmental modifications indicate need of
comprehensive assistive technology assessments, including child factors, family
factors, technology factors and service system factors.
Keywords: Assistive
devices, environmental modification, cerebral palsy, mobility
Introduction
Cerebral
palsy (CP) is the most frequent motor disability in childhood with a prevalence
rate about 2 – 2.5 per 1000 live birth [1,2]. These children can have many
neurological deficits that interfere with motor function and everyday
activities [3 – 7]. Traditionally, intervention for CP was based on impairment-oriented
models with the child as the only focus of intervention, denying the mediating
role of the environment on functioning. In paediatric rehabilitation today, the
environmental influences on development and disability are recognised.
Multidimensionalconcepts,
such as the International Classification of Functioning, Disability and Health (ICF)
advances the assumption that human functioning is a product of a person’s
interaction with the physical and social environment [8]. The concept of the
environment in the ICF includes both the immediate environment of a child
(e.g., products and technology, housing, and support fromthe family) and the
more distant environments (e.g., services, societal attitudes, and policies).
Facilitators are factors in a child’s environment that could improve
functioning,whereas
barriers are factors that through their presence or absence could limit
functioning.
Each
day a child must eat, groom, dress, maintain continence, change positions, move
around, climb stairs, understand requests, communicate basic needs, solve
problems, play, and interact with peers. A wide range of environmental
modifications, including assistive devices can be used to support performance
of daily activities. Assistive devices refer to any item, piece of equipment,
or product system that is used to increase, maintain or improve functioning in
people with disabilities [9]. Other environmental modifications such as grab
bars, ramps, lifts, and adaptations of home interiors or exteriors are often
delivered in conjunction with assistive devices. A unifying
characteristic of any modification is its purpose to modify the way a child
interacts with the immediate environment to maximize performance of daily life
activities. There are three pivotal points of performance for which
environmental modifications may be effective. The first point to the child’s functional
independence, defined as ability to perform essential tasks in the areas of
self-care, mobility and social function [10]. The second refers to the amount of
caregiver assistance required to perform these activities [11]. The third point
focuses on the demands associated
with the day-to-day caregiving to the child [12]. Service systems that take
part in provision of assistive technology need knowledge on how environmental modifications
affect these aspects of functioning in daily life.
There
is scarce systematic documentation of use and benefits of assistive devices and
other alterations for everyday activities in children with disabilities. In a
regional study, Korpela et al. [13] found that 77% of the families benefited
from use of assistive devices for bathing, eating, dressing and toileting. The
most common diagnosis in the study was CP. In CP, research has focused on the
functional impact of single devices, such as adaptive seating and powered wheelchairs
[14 – 18]. Thus, there is a lack of studies that describe the wide range of
environmental modifications that are used for daily activities. The aim of the
present study was to describe all assistive devices and other environmental
modifications provided to support everyday activities in young children with
CP, and the benefits of these modifications for functioning and caregiving. We
posed the following questions:
How
are types and numbers of environmental modifications distributed across
activity areas of
mobility,
self-care and social function?
What
is the impact of environmental modifications on functional independence and
care?
Methods
Sample population
This
study followed a cross-sectional design. The participants were recruited from
five counties in south-east
Measurements
The
Gross Motor Function Classification System (GMFCS) [19] was used to classify
severity of CP. The GMFCS classify limitations in gross motor function at five
severity levels, from level I with least limitations to level V with most
limitations. Distinctions between the five levels are based on functional
limitations and need for assistive mobility devices. To accommodate the
changing functional disabilities at different ages, the system describes gross
motor function for four age bands: less than 2 years, 2 – 3 years, 4 – 5 years,
and 6 – 12 years. A summary of the expected gross motor function for children 6
– 12 years for each level is provided in Appendix I. The GMFCS has established
validity and reliability [19 – 21].
The
PEDI [11] was used to measure functioning in mobility, self-care and social
function using the three measurement scales: functional skills, caregiver assistance,
and modifications. The Functional Skills scale includes 197 activities from all
the nine domains of the activity and participation dimension of the ICF [22],
measuring if the activities can be performed or not (scored 1/0). The Caregiver
Assistance scale assesses the required amount of help in seven areas of
mobility, eight areas of self-care, and five areas of social function using a
six point scale (see Appendix II). Summary scores are transformed into scaled
scores (0 – 100) that provide an estimate of the child’s achievements of
activities and amount of assistance. Both the Functional Skills and the
Caregiver Assistance scale measure functioning with use of environmental
modifications. The Modification scale is a frequency count of alterations to
support performance in the same areas as for caregiver assistance. The PEDI has
established validity and reliability [11,23 – 26].
The
Classification of Technical Aids for Persons with Disabilities (ISO 9999) [27]
was used to classify the environmental modifications. In this system, the products
are classified according to their principal 850 S. Østensjø et al. function.
Non-technical solutions are not included in this
classification. In
Data collection
Parents
(and the primary caregiver of the two children in residential care) completed
questionnaires collecting information about sociodemographic factors and
associated problems (such as epilepsy, learning difficulties and visual problems),
before the parent interview.
Nappies
and fences in use after 4 years of age were coded as assistive aids, because
few non-disabled children use this equipment regularly after this age. Preliminary
inspections of the data showed that use of environmental modifications was
identical for some activity areas and led to the decision that these areas
could be combined or excluded. Dressing upper and lower body and also
functional comprehension and expression were combined to one area. Problem
solving was excluded because modifications used for communication covered this area.
The number of modifications per child was counted for each of the remaining 17
areas. To sum up the use within the domains, any modification used across areas
was only counted once. Statistical analyses were performed with the
Results
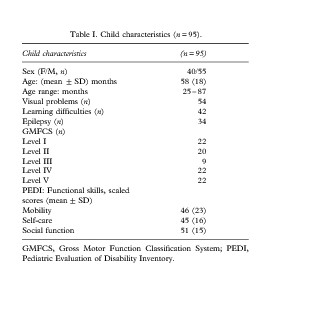
Characteristics of the children and their caregivers Main characteristics of the children and their disabilities are presented in Table I. The children’s need of caregiver assistance varied a lot across the activity areas of the PEDI, ranging from independent to totally dependent on help (Figure 1). In mobility, many children could move independently indoors whereas they needed a great amount of assistance for transfer activities. The children required extensive help in all areas of self-care, except for eating. Amount of assistance was more evenly distributed across the areas of social function.
Eighty-seven
children lived with two parents/caregivers, six with their mothers and two in residential
care. Most parents were born in
Overall use of environmental
modifications
Eighty-six
of the 95 children were provided with 1497 environmental modifications from the
National Insurance Scheme; assistive devices and other alterations for everyday
activities (n=1075), aids for therapy and
training (n=299), and orthopaedic devices (n=123).
The present study includes the 1075 modifications, which were provided to
enhance everyday functioning among 84 children. About 9% were not in regular
use. Thus a total of 980 modifications were used to support mobility, self-care
and social function. The main reasons for limited use could be grouped in four
categories. The first category referred to no or minimal need of the present
device or need of a more appropriate aid. The phrase ‘no or limited need’ was
often used for eating utensils, and the phrase ‘need of a more appropriate aid’
was frequently used for toilet and bathing
equipment that did not fit the child. The second category was related to time demand
and handling
of the child. Devices for transfer was perceived as less practical and more
time-consuming than lifting the child, and communication aids as less natural
than using personal signs and gestures. The third category referred to housing conditions
and transportation that hindered functional use of equipment in the bathroom
and devices like walkers and powered mobility. The last category pointed at
lack of immediate and ongoing training of the child and the parents for
effective use of powered mobility, alternative communication, computers and
toys.
In
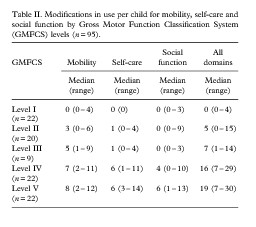
general, use of environmental modifications increased
with GMFCS levels (Table II). The variations within the severity levels were
large, except for level I, in which few modifications was used. As much as 80%
of the modifications were found among children at levels IV and V. Numbers in
use did not differ significantly between these two severity groups. Further
comparisons showed that children at level II used more modifications than
children at level I in all domains (Mann – Whitney U-test,
P=0.001 to 0.042). No significant difference appeared
between children at levels II and
Use of modifications across areas of
mobility, self-care and social function
Frequency
and number of modifications in use across the activity areas of mobility,
self-care and social
function are shown in Table
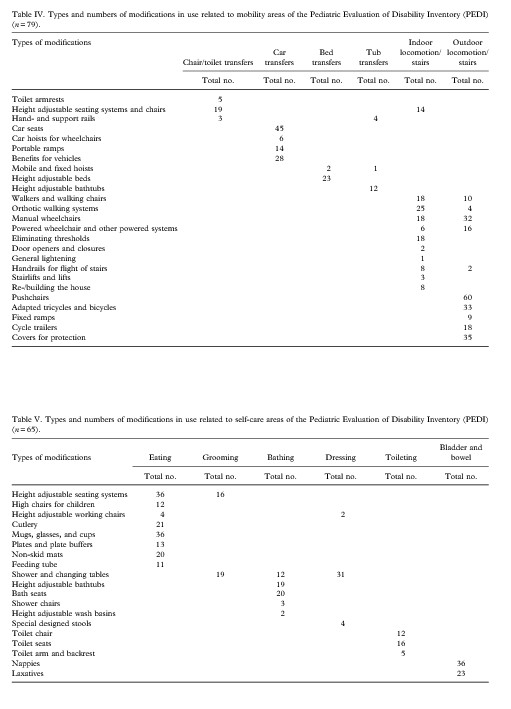
Mobility
The
440 environmental modifications used for mobility were classified in three
classes and 27 categories
of the ISO 9999. Grants for vehicles and rebuilding houses are not classified
in this system. About 20 modifications were not in use; these were manual and
powered wheelchairs, orthotic walking systems, tricycles, hoists, and portable
ramps. Table IV shows the types of modifications in use related to the areas of
mobility. Environmental modifications for mobility could
be grouped in two categories: (1) mobility devices and (2) modifications of
housing and transportation. The most commonly used mobility devices were
walkers, manual and powered wheelchairs, tricycles, push-chairs, seating
systems and car seats. Eight children used their walking system or powered wheelchair
only at kindergarten or school because of housing or transportation conditions.
Twenty-nine families have made some modifications of their housing such as
elimination of thresholds, extra handrails for flights and stairs, alterations
related to bathrooms,
ramps, and a new or larger terrace. Further, 28 children had received grants to
get a suitable
van for transportation of the child and the mobility devices. However, twenty
parents reported that the physical environment hindered incorporation of
mobility devices into their daily routines.
Self-care
The 340 environmental modifications that were used to assist self-care activities were classified in four classes and 17 categories of the ISO 9999. Feeding tubes, nappies and laxatives are not classified in this system. About 40 assistive devices were not in use. The abandoned devices were cutlery or cups for eating, shower chairs and bath seats, stools for dressing, and toilet equipment. Table V shows the types of modifications in use related to the areas of self-care. A large number of devices, such as adaptive seating, eating and drinking utensils, and feeding tubes were used for eating. Adjustable seating systems and shower and changing tables were frequently used across activity areas. Bathing and toilet equipment were most often abandoned. Seven shower chairs and the same number of bath seats were not in regular use. Six toilet seats and eight toilet chairs were not used, although they were needed to improve bladder and bowel management. As many as 36 of the 63 children that had passed their fourth birthday used nappies, and 23 children used laxatives regularly.
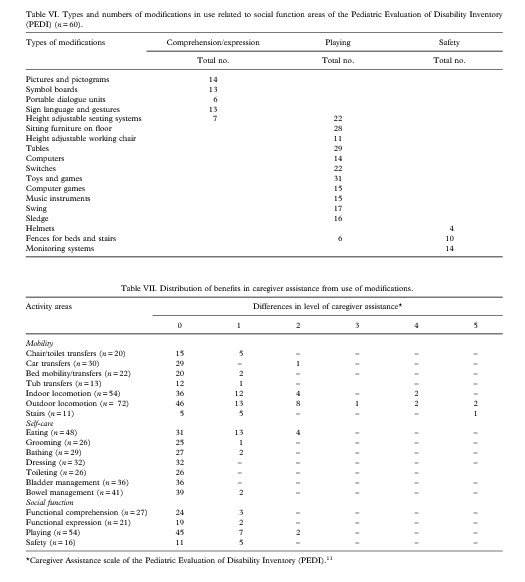
Social functionThe 287 environmental modifications used to support social function belonged to five classes and 18 categories of the ISO 9999. Sign language and gestures are not classified in this system. About 35 modifications were not in regular use. The non-used devices were aids for communication, sitting furniture, tables, computers, switches and toys for playing. Table VI shows the types of modifications in use related to the areas of social function. Twenty-one of the 35 children with severe limitations in communication used alternative or augmentative methods to support receiving messages and for expression. These methods could be grouped in two categories: (1) personal signs and gestures and (2) communication aids. Half of the communication aids was used only in kindergarten or school. Adapted seating was frequently used to increase sitting stability when playing with toys or on the computer. Playing activities were modified with use of switches to control objects, battery-activated toys, and adapted toys and games.

Impact of modifications on functional
independence and care
Strong
to moderate correlation was seen between amount of caregiver assistance and
number of modifications
in use for mobility, self-care and social function (rs=
0.78, 0.65 and 0.60, P50.001, respectively).
Substantial reduction in need of caregiver assistance with use of modifications
was reported
mainly for indoor and outdoor mobility, and eating (Table
The
parents’ ratings of the impact of the modifications on functional independence
and caregiving complemented
these findings (Figure 2). To investigate how functional independence was
related to care demands in mobility, self-care and social function, the data of
the impact of modifications were
dichotomised into benefits (moderate to very large impact) and no benefits (no
or minor impact). In all domains, there was a strong association between the
child’s independence and caregiver demands (w2 =
9.8 – 60.0, df = 1, P=0.002 to 50.001).
For
mobility, about half of the 79 parents rated the modifications to have moderate
to very large effect on the child’s functioning, and two-thirds reported similar
effects on caregiver demands. The largest benefits were seen for children at
GMFCS level IV, for which modifications improved mobility in 18 users and
facilitated care in 19 of the 22 users. In the 22 users at level V,
modifications lightened care in 18 and improved functioning in half as many.
Seven out of
17 users at level II and four out of nine users at level
For
self-care, four out of five parents (n=65)
reported no or minor effect of the alterations on the child’s
performance, whereas three out of four judged the modifications to facilitate
the care, at least
moderately. Modifications improved self-care skills in nine of the 22 users at
GMFCS level IV and facilitated care in 17 users. No user at level V improved
their skills, whereas the modifications lightened caregiving in 19 of the 22
users. Out of seven users at level
For
social function, the benefits were generally low. One out five parents (n=60)
reported positive effects
from the modifications. Benefits occurred in parallel for the child’s
functional independence and caregiver demands. Five users out of 21 at level
IV, four users out of 22 at level V, and only two users out of 17 at levels I –
Discussion
The results showed frequent use of environmental modifications to support everyday activities. High proportions of the provided modifications were in use and functioned properly. The extent of use and non-use was within the range of previous reports in children [30,31]. Use of modifications increased with GMFS levels, and most of the modifications were applied among children at levels IV and V. This result support that severity of gross motor limitations is closely associated with use of assistive devices and other environmental modifications for daily activities [13].
Results
from impact of modifications on functional independence and caregiving
discoveredinteresting
differences for mobility, self-care and social function. With regard to
mobility, the benefits were significant for both functioning and care. For indoor
and outdoor locomotion, half of the caregivers reported reduced amount of
assistance by one or more levels on the Caregiver Assistance scale under the
environment-adjusted conditions. The same amount perceived that devices such as
orthotic walkers, powered mobility and adapted bikes had improved the child’s
overall mobility. These findings show that specific mobility devices can offer
children with severe limitations in self-mobility alternative means of
independent mobility. Wright et al. [32] observed that 11 of the 20 studied
children with severe CP succeed to walk at least 30 metres with an orthotic
walker, while the rest partially completed the distance after 12 months
training. Bottos et al. [14] reported that 21 of 27 of children with severe
motor deficiency were able to operate a powered wheelchair with little or
minimal assistance after a 6 – 8-month training. Other devices such as movable
seating systems, pushchairs and manual wheelchairs were listed to facilitate
care. Pushing the child in a device represents an alternative mean of dependent
mobility that
implies less physical strain than carrying the child.
In
contrast to the considerable benefits of mobility devices, the benefits of
devices for transfer were limited. Equipment such as hoists, portable ramps, and
height adjustable technology was often in irregular use, and using them seemed
less practical and more time-consuming than lifting the child. Statements like
‘we have to use them when she gets heavier’ and the high level of caregivers
assistance for transfer activities, indicate that transfer in and out of chairs,
toilet, bed, bathtub, and car are critical activities for care burden, and
therefore need to be focused during childhood.
The
usability of devices for mobility and transfer seemed to be related to housing
and transportation conditions. About one third of the families had done some
modifications of their home and/or van, yet many still experienced physical
barriers in the immediate environment. These results support previous findings
that more attention must be paid to housing and transportation circumstances to
support independence and care in children with motor disabilities
[33,34].
For
self-care, the impact of the modifications on caregiving was much larger than
the impact on functional
independence. Most children required extensive assistance to perform self-care
activities. Eating was the only area which modifications could reduce the
amount of assistance. Beneficial effects were reported for adjustable seating
systems and eating and drinking utensils. These finding support previous
studies that adaptive seating could improve eating abilities and reduce
caregiver support in some children with limitations in sitting [16,17].
However, small improvements in self-feeding and drinking skills can lead to
increased feeding time [18]. Impaired oral-motor function is a another common feature
of children with severe CP, which can be associated with extended feeding time,
fatigue during eating, food refusal and malnutrition [35,36]. Use of feeding
tubes appeared to reduce care burden. Statements like ‘no longer pressing the
child to eat more and faster’ suggest reduced intensity of care and greater
satisfaction with the feeding process. However, all the parents remarked that
tasting food or
eating part of the meals orally was important for the stimulation and the
interaction with the child.
Postural
support devices that function properly seemed to be essential for functional
ndependence and care in many daily activities [16,17,37]. Dissatisfaction and
non-use of toilet equipment, that was needed, demonstrate the difficulties of
finding a device that fit the child and the activity [37]. Frequent use of
nappies after 4 years of age and laxatives support that urinary incontinence
and constipation is a major issue in the basic care of many children with CP
[37,38]. The need of toilet equipment was also confirmed by high return to the Assitive
Technology centres and provision of other models. Inadequate sitting comfort
and discomfort when seated are likely explanations for the bad match between
the child and toilet devices. Zhang et al. [39]
suggested that comfort and discomfort are different but related entities.
Whereas comfort is associated
with relaxation and well being, discomfort is associated with fatigue and
biomechanical factors. Toilet systems that fall in short in addressing positioning
needs could hinder toilet training [37]. Using the ICF classifications: body
functions (b), Activities and Participation (d), and environmental factors (e)
[8], we showed that lack of appropriate toilet
equipment (e 1151)* was a barrier for bladder and
bowel management (d5300 and d5301) that could lead to increased bladder
problems and constipation (b620 and b525).
For
social functions, fewer parents experienced positive impact of modifications on
both functional independence and care. This finding indicates that it may be
more difficult to capture the effect of modifications because of the complexity
of activities such as communication and playing. Many of the functionally
non-speaking children did not use alternative or augmentative communication.
Limited use could be due to our categorisation of alternative communication,
not including facial expression and body movements that are usual modes of
communication for
children with severe expressive impairments [40]. Another reason could be the children’s
difficulties to produce consistent and readable movements and vocalisation
[41]. The result that half of the provided communication aids were used in
kindergarten and schools, and not at home,
indicate that parent – child communication was dominated of natural methods,
such as vocalisation, signs, and gestures. Communication with aids requires new
skills of the caregivers and developing of positive attitudes toward the
devices [42,43]. Incorporation of communication aids into everyday life call
for involvement of the families in development of communication systems and in
ongoing training.
The
Caregiver Assistance scale showed high parental participation in playing.
Parents of children with
disabilities have to mediate the environment to let the child learn through
active exploration and interaction with materials and other children [49]. Providing
the child with adequate toys and devices is only one among several contextual
factors that can influence playing. Positioning the child, the toy itself, how
to interact and use material, attitudes, and limited time because of the
child’s other needs are all factors that could explain the relatively small
benefits of modifications [49 – 51]. However, we are in lack of knowledge on
how playing material interact with other contextual and personal factors to
facilitate social interaction and play in children with severe motor
and cognitive impairments.
Conclusions
The
study documented a clear relation between use of environmental modifications
and GMFCS levels. The modifications were distributed across the activity areas
of the PEDI, however there were considerable variations in use and benefits.
Functional independence and caregiving demands often benefited from different
types of assistive devices. Matching devices with the child, the activity and
the caregivers was identified as a challenge. Furthermore, more attention must
be paid to housing and transportation circumstances to support use of assistive
devices.
The
results suggest use of the GMFCS for planning of assistive technology services
and the PEDI
to describe the use of environmental modifications for everyday activities.
Since the PEDI measures
functioning including modifications, other tools are needed to assess the
effect of environmental changes. The parents had a great deal of impact on use
and benefits and need to be involved in comprehensive assistive technology
assessments including child factors, family factors, technology factors and
service system factors. Evaluation of needs, use and benefits of modifications
is an ongoing process that should be integrated into rehabilitation plans for
children with moderate to severe CP.
The
study was limited in being cross-sectional and descriptive. The results need to
be expanded upon within studies designed to examine the specific influence of
modifications, using a multidimensional concept, such as the ICF. Additional
qualitative studies would help us to better understand the observed differences
in use and benefits of modifications.
Acknowledgements
We
are grateful to all the children and the parents who participated. We
acknowledge the contribution of the assistive technology centres and the
habilitation centres in Akershus, Buskerud,
References
1.
Hagberg B, Hagberg G, Beckung E, Uvebrandt P. Changing panorama of cerebral
palsy in Sweden.VIII. Prevalence and origin in the birth year period 1991 – 94.
Acta Paediatrica 2001;90:271 – 277.
2.
Surveillance of Cerebral Palsy in
3.
Lepage C, Noreau L, Bernard P-M, Fougeyrollas P. Profile of handicap situations
in children with cerebral palsy. Scandinavian J of Rehabilitation Medicine
1998;30:263 – 272.
4.
Østensjø S, Carlberg EB, Vøllestad NK. Everyday functioning in young children
with cerebral palsy: functional skills, caregiver
assistance, and moficiations of the environment. Developmental Medicine &
Child Neurology 2003;45:603 – 612.
5.
Østensjø S, Carlberg EB, Vøllestad NK. Motor impairments in young children with
cerebral palsy: relationship to gross motor
function and everyday activities. Developmental Medicine & Child Neurology
2004;46:580 – 589.
6.
Barabas G, Matthews W, Zumoff P. Care-load for children and young adults with
severe cerebral palsy. Developmental Medicine
& Child Neurology 1992;34:979 – 984.
7.
Roberts K, Lawton D. Acknowledging the extra care parents give their disabled
children. Child: Care, Health and Development 2001;27:307 – 319.
8.
World Health Organization. International Classification of Functioning,
Disability and Health (ICF). Geneva: World Health
Organization; 2001.
9.
The Technology-Related Assistance for Individuals with Disabilities Act. Pub.
L. No. 100 – 407, 1988.
10.
Msall ME, Tremont MR, Ottenbacher KJ. Functional assessment of preschool
children: optimizing developmental and
family supports in early intervention. Infants and Young Children 2001;
11.
Haley SM, Coster WJ,
12.
Floyd FJ, Gallagher EM. Parental stress, care demands, and use of supportive
services for school-aged children with disabilities
and behavior problems. Family Relations 1997;46:359 – 371.
13.
Korpela RA, Seppa¨nen R-V, Koivikko M. Technical aids for daily activities: A
regional survey of 204 disabled children. Developmental
Medicine & Child Neurology 1992;34:985–998.
14.
Bottos M, Bolcati C, Sciuto L, Ruggeri C, Feliciangeli A. Powered wheelchairs
and independence in young children with
tetraplegia. Developmental Medicine & Child Neurology 2001;43:769 – 777.
15.
Butler C. Effects of powered mobility on self-initiated behaviours of very
young children with locomotor disability. Developmental
Medicine & Child Neurology 1986;28:325 – 332.
16.
Reid D, Rigby P, Ryan S. Functional impact of a rigid pelvic stabilizer on
children with cerebral palsy who use wheelchairs: users’ and caregivers’
perceptions. Pediatric Rehabilitation 1999;3:101 – 118.
17.
Rigby P, Reid D, Schoger S, Ryan S. Effects of a wheelchairmounted rigid pelvis
stabilizer on caregiver assistance for children
with cerebral palsy. Assistive Technology 2001;13:2 – 11.
18.
Roxborough L. Review of the efficacy and effectiveness of adaptive seating for
children with cerebral palsy. Assistive Technology 1995;
19.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development
and reliability of a system to classify gross motor function in children with
cerebral palsy. Developmental Medicine & Child Neurology 1997;39:214 – 223.
20.
Bodkin AW, Robinson C, Perales FP. Reliability and validity of the Gross Motor
Function Classification System. Pediatric Physical Therapy, 2003;15:247 – 252.
21.
Wood E, Rosenbaum P. The Gross Motor Function Classification System for
Cerebral Palsy: a study of reliability and
stability over time. Developmental Medicine & Child Neurology 2000;45:292 –
296.
22.
Bjorbækmo W. Kartlegging: et spørsma˚l om perspektiv og projeksjon [Assessment:
a question of perspectives and projection].
(Master thesis).
23.
Feldman AB, Haley SM, Coryell J. Concurrent and construct validity of the
Pediatric Evaluation of Disability Inventory. Physical
Therapy 1990;70:602 – 610.
24.
Haley SM, Coster WJ, Faas RM. A content validity study of the Pediatric
Evaluation of Disability Inventory. Pediatric Physical
Therapy 1991;3:177 – 84.
25.
Nichols DS, Case-Schmidt J. Reliability and validity of the Pediatric
Evaluation of Disability Inventory. Pediatric Physical Therapy 1996;
26.
Wright FV, Boschen KA. The Pediatric Evaluation of Disability Inventory (PEDI):
Validation of a new functional assessment
outcome instrument. Canadian J of Rehabilitation 1993;
27.
European Committee for Standardization. Technical aids for persons with
disabilities – Classification and terminology (ISO 9999). Brussel: European
Committee for Standardization; 2002.
28.
National Insurance Administration. The provision of assistive aids – a part of
a larger system. Information about provision of assistive aids.
29.
Jahnsen R, Berg M,
30.
Korpela RA, Seppa¨nen R-V, Koivikko M. Rehabilitation service evaluation: a
follow-up of the extent of use of technical aids for disabled children.
Disability and Rehabilitation 1993;15:143 – 150.
31.
McGrath PJ, Goodman JT, Cunningham SJ, MacDonald B-J, Nichols TA, Unruch A.
Assistive devices: utilization by children.
Archives of Physical Medicine and rehabilitation 1985;66:430 – 432.
32.
Wright FV, Belbin G, Slack M, Jutal K. An evaluation of the David Hart Walker
orthosis: a new assistive device for children with cerebral palsy.
Physiotherapy
33.
Korpela RA. A regional survey of the housing circumstances of families with
children experiencing intellectual and motor disabilities. Disability and
Rehabilitation 1992;14:176 – 182.
34.
Wiart L, Darrah J, Cook A, Hollis V, May L. Evaluation of powered mobility use
in home and community environments. Physical
& Occupational Therapy in Pediatrics 2003;
35.
Samsong-Fang L, Butler C, O’Donnell M. Effects of gastrostomy feeding in
children with cerebral palsy: an AACPDM report. Developmental Medicine & Child Neurology 2003;45:412
– 16.
36. Del Giudice E, Staiano A, Capano G,
Romano A, Florimonte L, Miele E, Ciarla C, Campanozzi A, Crisanti A.
Gastrointestinal manifestations in children with cerebral palsy. Brain
and Development 1999;21:307 – 31.
37.
Lee DF, Ryan S, Polgar JM, Lebel G. Consumer-based approach used in development
of adaptive toilet system for children
with positioning problems. Physical and Occupational Therapy in Pediatrics
2002;22:5 – 24.
38.
Bosch, J, Mraz R, Masbruch J, Tabor A, Van Dyke D, McBrian D. Constipation in
young children with disabilities. Infants
and Young Children 2002;15:66 – 77.
39.
Zhang L, Helander MG, Drury CG. Identifying factors of comfort and discomfort
in sitting. Human Factors and Ergonomics
Society 1996;38:377 – 399.
40.
41.
Calculator SN. Use of enhanced natural gestures to foster interactions between
children with Angelman syndrome and their
parents. American J of Speech-Language Pathology 2002;11:340 – 355.
42.
Parette, HP Jr, Brotherson MJ, Huer MB. Giving families a voice in augmentative
and alternative communication decision-making. Education and Training in Mental
Retardation and Developmental Disabilities 2000;35:177 – 190.
43.
Fallon KA; Light JC, Page TK. Enhancing vocabulary selection for preschoolers
who require augmentative and alternative
communication. American J of Speech-Language Pathology 2001;10:181 – 195.
44.
Besio S. An Italian research project to study the play of children with motor
disabilities: the first year of activity. Disability
and Rehabilitation 2002;24:72 – 9.
45.
Brodin J. Play in children with multiple disabilities: play with toys – a
review. International J of Disability, Development and Education 1999;46:25 –
34.
46.
Sullivan M, Lewis M. Assistive Technology for the very young: Creating
responsiveness environments. Infant and Young
Children 2000;
47.
Daniels LE, Sparling JW, Reilly M, Humphry R. Use of assistive technology with
young children with severe and profound
disabilities. Infant-Toddler intervention 1995;5: 91 – 112.
48.
Malone DM, Langone J. Teaching object-related play skills to preschool children
with developmental concerns. International J of Disability, Development and Education
1999;46:325 – 336.
49.
Fallon, MA, Harris MB. Factors influencing selecting of toys for handicapped
and normally developing preschool children. J of Genetic Psychology
1989;150:125 – 34.
50.
Lane SH, Mistrett SG. Play and assistive technology issues for infants and
young children with disabilities: a preliminary examination. Focus on Autism
& Other Developmental Disabilities 1996;11:96 – 106.
51. Malone DM. Contextual factors informing play-based program planning. International Journal of Disability, Development and Education 1999;46:308 – 324.